Health equity isn’t a one-size approach
The COVID-19 pandemic highlighted the crucial connection between Social Determinants of Health (SDOH) and patient outcomes. Addressing medical and behavioral health needs requires a comprehensive understanding of a patient’s social context.
Effective interventions and care plans must meet patients "where they are," and one-size-fits-all approaches fail to address diverse vulnerabilities and needs.
For healthcare organizations looking to begin or enhance their equity initiatives, the National Committee for Quality Assurance's (NCQA's) Health Equity Accreditation (HEA) is an excellent starting point. HEA is a comprehensive framework that aligns with many other recognized programs, such as those from the Joint Commission and CMS, providing a holistic approach to advancing health equity. It aims to improve the quality of care and patient experience within the United States.
3 Reasons why NCQA HEA is the perfect starting point
1. Alignment with patient-centered programs
NCQA integrates HEA deliverables into its broader patient-centered programs, weaving equity considerations into healthcare system delivery.
2. Framework for equitable care
NCQA offers organizations a seamless pathway. It helps cultivate an equitable culture and establish a framework for equitable medical care delivery. This framework ensures that all patients receive care tailored to their specific needs, reducing disparities and improving outcomes.
3. Applicability across the healthcare spectrum
The HEA program applies to more than insurance carriers. It also involves health plans, wellness organizations, population health entities, health systems, ACOs, practices, hospitals and more. This broad applicability makes it a versatile tool for various healthcare establishments.
Benefits of NCQA Health Equity Accreditation
Reducing Inequities
The HEA program supports efforts to reduce health disparities by promoting value-based contracting and incremental quality improvement. It helps align organizational structures to better address the needs of diverse populations through tailored workflows, resources, screenings and data analysis.
NCQA HEA Program Highlights
The HEA program focuses on several key areas to promote health equity:
Internal readiness: Ensuring diverse staffing, comprehensive training and inclusive practices within the organization.
Data collection & analysis: Collecting and analyzing diversity data (race, ethnicity, sexual orientation/gender identity, language) to identify and address gaps in care.
Language services: Implementing services for language translation and sharing practitioner language proficiencies with patients to ensure effective communication.
Culturally appropriate care: Sharing practitioner race and ethnicity data with patients to enhance culturally appropriate care.
Annual work plans: Developing annual work plans with goals, interventions and evaluations to ensure culturally and linguistically appropriate services.
Quality measures: Stratifying and analyzing quality measures by diversity to set and achieve incremental improvement goals, such as reducing health inequities.
In addition, NCQA has various health equity resources available to assist organizations.
Enhancing your equity efforts with NCQA Health Equity Accreditation Plus
For organizations that have achieved HEA, the NCQA Health Equity Accreditation Plus (HEA+) program offers additional benefits. Building on the foundational elements of HEA, HEA+ focuses on:
Social risk analysis: Conducting social risk analyses and creating mitigation plans to address SDOH within covered communities.
Community resource evaluation: Assessing community resources, identifying gaps and establishing interactive, bi-directional partnerships to address social needs.
Targeted programs: Developing programs with specific goals, governing bodies and time frames to mitigate and overcome social needs.
Take the guesswork out of NCQA accreditation
The NCQA programs offer a structured and comprehensive approach for healthcare organizations to advance their equity initiatives. By incorporating HEA and HEA+ into their operations, healthcare entities can ensure that they provide equitable, culturally competent care to all patients, ultimately improving health outcomes and reducing disparities.
Ready to start your health equity journey? Learn more about how DataGen’s Medical Practice Consulting service can help your organization achieve NCQAHEA/HEA+ goals and deliver equitable patient care. Contact us today to see how we can help you elevate your care.
If you’re a New York state healthcare establishment, discover how the New York state 1115 Medicaid Wavier could positively impact your practice.
Exciting news for New York state healthcare establishments!
As of April 1, 2024, NYS will provide additional incentives to Patient-Centered Medical Home (PCMH) recognized practices. By treating each patient and their individual needs, NYS aims to recognize cost reductions, satisfaction increases and outcome improvements. For PCMH providers, it is more rewarding than ever to take advantage of these patient-focused programs to understand how to serve patients holistically.
NYS 1115 Medicaid Waiver Enhanced Payments
Under the NYS 1115 Medicaid Waiver, primary care practices with PCMH recognition from the NCQA are eligible to receive increased Medicaid Incentive Payment.
As of April 1, sites will receive:
$4 enhanced payment for patients 0-22 years.
$2 enhanced payment for patients 23+ years.
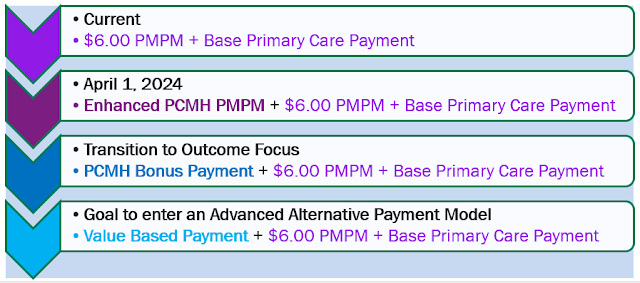
This equates to either $10 or $8 dollars in total Per Member Per Month (PMPM). The payment progression is outlined below.
If you’re participating in PCMH, consider adding HEA accreditation
This positively impacts your patients; eventually, the enhanced payments will migrate to outcome-focused payments. The stronger your practice foundation, the more seamless it will be to maintain increased revenue.
Along with NCQA HEA/HEA+ accreditation, DataGen can help you achieve PCMH recognition. Explore our Medical Practice Consulting solution to see how we can help advance your practice and earn enhanced payments.

.jpeg)
Comments
Post a Comment