Accurate and standardized healthcare data are essential for informed decision-making and compliance. In New York state, the Statewide Planning and Research Cooperative System (SPARCS) plays a critical role in collecting and analyzing patient data. Central to this system is the SPARCS data dictionary, a comprehensive resource that ensures consistency in data reporting across healthcare providers. This blog will explore the SPARCS data dictionary, including:
key components and practical applications;
how it can streamline healthcare operations; and
how understanding it can simplify your submission routines.
We will also cover SPARCS data automation and DataGen’s automated SPARCS data submission tool, UDS (UIS Data System™), and how it can help you achieve 100% accuracy and compliance with minimal effort.
Who should use this SPARCS data dictionary?
Key roles in ambulatory surgery centers (ASCs)
This SPARCS data dictionary is a valuable resource for ambulatory surgery centers (ASCs) looking to streamline their data submissions and maintain compliance with New York state reporting requirements.
Whether you're a practice administrator or an office manager, having a clear understanding of SPARCS data elements can help you ensure accuracy, reduce errors and improve reimbursement efficiency. By leveraging this resource, ASCs can simplify the complexities of data reporting, avoid compliance pitfalls and enhance overall operational effectiveness.
Professionals in key administrative roles, such as managing administrators, business office managers and managers, will also find this SPARCS data dictionary essential for optimizing data workflows. With accurate SPARCS reporting playing a crucial role in financial and regulatory success, these leaders can use the dictionary to standardize processes, enhance team training and proactively address data submission challenges. Whether you're overseeing daily operations or managing revenue cycle processes, this guide can help you navigate SPARCS data requirements with confidence.
What is the SPARCS data dictionary?
The SPARCS data dictionary serves as a standardized guide for healthcare providers to report data to New York’s Statewide Planning and Research Cooperative System (SPARCS). It outlines the defined data fields, formats and codes when submitting patient information.
The dictionary helps us better understand the data extracted from SPARCS and how it relates to the data submitted.
SPARCS data dictionary encompasses a wide range of information, including:
patient demographics;
diagnoses and procedures (using ICD-10 and CPT codes);
admission and discharge details; and
billing and financial data.
This robust dataset supports research, policy development and financial planning across New York’s healthcare landscape. The New York State Department of Health oversees SPARCS submissions to ensure that the data meet rigorous standards for public health use and policy implementation.
Key SPARCS terms and definitions
To better understand how to work with SPARCS data, it is important to familiarize yourself with common terms and definitions. Below are some key terms describing data collected based on the SPARCS glossary:
Ambulatory surgery services: Procedures performed on an outpatient basis at Article 28 facilities.
De-identified data: Data that have been stripped of personal identifiers to protect patient privacy while still being useful for research and analysis.
Data element: The smallest unit of information that provides meaningful data, such as patient date of birth or gender.
Data Use Agreement (DUA): A formal agreement outlining the conditions under which SPARCS data may be accessed and used.
Emergency department services: Care provided in an emergency department, including diagnostic and therapeutic services.
Identified data: Data that include personal identifiers and are subject to stringent access controls.
Outpatient services data: Information related to services provided to patients who are not admitted to the hospital.
Department of Health (DOH): The governing body responsible for overseeing SPARCS compliance and operations in New York.
4 Core SPARCS data dictionary components
1. Data fields
The SPARCS data dictionary focuses on SPARCS output. Identifiers and data elements are critical for comprehending trends and delivering actionable insights. Understanding what is being reported clarifies the fields needed for a record to pass SPARCS edits. This includes patient identifiers, insurance details, clinical information and inpatient discharges.
Examples of a SPARCS data field
Admission Date (ADMIT_DT): Date of admission or start of care.
Date of Service (SVC_DT): Date of service provided.
Claim FROM Date (CLM_FROM_DT): Statement from Date Beginning date of the billing period.
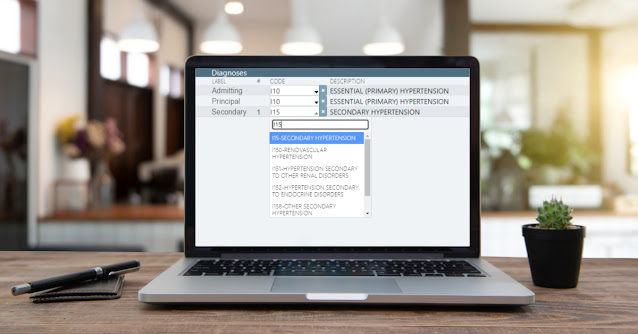
2. Format and coding standards
The dictionary provides detailed guidelines on acceptable data formats, ensuring uniformity in submissions. It also outlines coding standards, such as:
ICD-10 codes: For diagnoses.
CPT codes: For procedures.
These standards are crucial for both inpatient and outpatient services data, including emergency department services and ambulatory surgery services.
3. Codes and values
Each data element includes specific codes and values. For instance, in the SPARCS data dictionary you can find several output data elements, including:
Race codes: Categorize patient race for demographic analysis.
Ancillary Total Charges (CHRG_ANCIL_AMT): Total of line charge amounts for ancillary revenue codes (codes not beginning with "01").
Patient Marital Status (PAT_MRITL_STS): Code indicating the patient's marital status.
Source of Payment Typology (PAYR_TYPOLOGY_CD): Code indicating the source of payment typology for this payer.
Provider NPI (PROV_NPI): Service provider's National Provider ID (NPI).
4. Version updates
Regular updates to the SPARCS data dictionary reflect changes in regulatory requirements, coding practices and reporting needs. Staying current with these updates is crucial for compliance. DOH regularly communicates updates to ensure healthcare facilities remain aligned with the latest standards.
Why the SPARCS data dictionary matters
Compliance
Healthcare organizations must adhere to SPARCS requirements to avoid penalties and maintain funding eligibility. The SPARCS data dictionary is the cornerstone of compliance, offering clear guidelines for accurate submissions.
Data accuracy
Standardized reporting minimizes errors and ensures that data are reliable for analysis and reporting. For example, emergency department data and outpatient visits must be reported consistently to enable effective resource allocation. Explore how you can overcome outpatient visit coding challenges for improved SPARCS compliance.
Operational efficiency
By following the SPARCS data dictionary, organizations can streamline data submission processes, saving time and resources. It also ensures smoother integration with data platforms used for public health initiatives, including Health Data NY.
SPARCS data dictionary challenges
Despite its importance, using the SPARCS dictionary can be challenging:
Complexity: Interpreting detailed requirements and updates can be daunting. Facilities such as Article 28 facilities, which provide ambulatory surgery services and emergency department services, often face challenges in ensuring data accuracy.
Integration: Incorporating SPARCS guidelines into existing data systems may require significant effort, especially for organizations transitioning to new data platforms.
Temporality: Data reporting priorities, standards and documentation have varied over SPARCS’ decades of existence. Keeping track of these changes requires dedication, persistence and strong organizational skills.
Solutions
Tools like automated validation systems and expert support can simplify the process.
Staying informed through training and updates is also essential.
Establishing a data governance committee can help healthcare organizations oversee SPARCS data submissions effectively.
SPARCS dictionary benefits
The SPARCS data dictionary is an indispensable tool for healthcare organizations in New York. Ensuring standardized, accurate and compliant data submissions empowers providers to meet regulatory requirements and leverage data for improved decision-making. From outpatient visits to inpatient discharges, the SPARCS system provides actionable insights that enhance public health outcomes and operational efficiency.
Practical applications of the SPARCS data dictionary
The SPARCS data dictionary has numerous applications in healthcare:
Policy development: Researchers and policymakers use SPARCS data to identify trends and craft informed healthcare policies. For example, de-identified data from outpatient services can provide insights into community health needs.
Operational planning: Hospitals and clinics analyze SPARCS data to optimize patient care and resource allocation, including emergency department services.
Financial management: Accurate data support revenue cycle management and compliance audits. A robust data use agreement ensures that all stakeholders adhere to ethical data practices.
SPARCS also facilitates the integration of its data into broader public health initiatives, enabling DOH to monitor statewide trends and address disparities effectively.
Data governance and SPARCS
Effective use of the SPARCS data dictionary relies on strong data governance practices. A data governance committee ensures compliance, oversees updates and manages the integration of identified and de-identified data. This plays a critical role in enabling healthcare organizations to leverage SPARCS data for strategic planning and quality improvement.
SPARCS data automation: What to know
Now that you understand SPARCS, its data dictionary and its challenges, here's what you need to know about SPARCS data automation and DataGen's SPARCS submission tool, UDS (UIS Data System™). It is the only SPARCS data automation solution available in New York state that manages data dictionary submission requirements for you.
Avoid preventable data scenarios and compliance risks
DataGen SPARCS automation is a game-changer in mitigating risks associated with preventable SPARCS data errors and compliance issues.
From acquisition challenges to evolving regulatory updates, DataGen’s solution ensures healthcare facilities stay ahead. Automated tools flag potential data inaccuracies — whether it’s missing identifiers, inconsistent data elements, or gaps in emergency department services reporting — before submissions are finalized.
This proactive approach reduces administrative burdens and minimizes the risk of penalties tied to non-compliance.
By integrating seamlessly with existing data platforms, DataGen helps facilities meet SPARCS submission requirements with confidence, enabling providers to focus on strategic priorities like improving public health outcomes and optimizing resource allocation.
The benefits of partnering with DataGen
Implementing SPARCS data automation makes the complex process of data submission simpler and more efficient. Here are the key benefits of automated SPARCS data submissions:
Automated compliance checks: DataGen’s solution automatically validates SPARCS submissions against the latest state requirements, ensuring accuracy and reducing the risk of penalties.
Streamlined integration: The platform seamlessly integrates with existing data systems, supporting both inpatient and outpatient services data, including ambulatory surgery and emergency department services.
Real-time error resolution: Errors in SPARCS submissions are flagged in real time, allowing healthcare organizations to address issues promptly before submission deadlines.
Enhanced reporting capabilities: With advanced analytics, DataGen’s automation tools enable organizations to gain deeper insights into trends, improving operational planning and resource allocation.
Expert support: DataGen provides access to a team of SPARCS experts who assist with troubleshooting and staying updated on regulatory changes.
By adopting DataGen’s SPARCS automation tools, healthcare providers can focus on delivering quality care while ensuring compliance and operational efficiency.
Ready to unlock DataGen’s UDS solution?
Navigating SPARCS submissions doesn’t have to be overwhelming. DataGen’s UDS (UIS Data System™) solution simplifies the process with automated compliance checks, seamless integration and expert support. Contact us to learn more about how our solution can help your organization excel in SPARCS reporting.
This content is for informational purposes only. It has been partially generated from an AI language model, which may not always be exhaustive or tailored to individual circumstances. We encourage you to contact one of our experts for more information. We assume no liability arising from any use of this content.

Comments
Post a Comment