What are the hallmarks of an effective public health department? Public health accreditation may not be the first answer that comes to mind. But the Public Health Accreditation Board created a framework that can help health departments transform their quality, accountability and performance.
The Community Health Assessment anchors the PHAB framework, which includes 10 Essential Public Health Services aligned to 10 domains and eight key public health capabilities. To improve your application process, it’s essential to see how your CHA affects your public health accreditation. These are the five things you need to know now.
1. Accreditation is prevalent but takes time
Per the CDC, 80% of state public health departments are PHAB accredited, as are hundreds of local and tribal agencies. These achievements didn’t happen overnight. Public health departments may lack the time, staff, data and partnerships to refine their CHAs, much less leverage them for accreditation.
Prior to accreditation and re-accreditation, the PHAB framework includes:
- Readiness Assessment — Completed before accreditation efforts can begin.
- Pathways Recognition — Achieved when full accreditation is not yet within reach.
2. The Essential Public Health Services are central to the CHA and PHAB accreditation
The CHA and PHAB accreditation help public health departments align with the CDC's 10 Essential Public Health Services:
- Assess and monitor population health.
- Investigate, diagnose and address health hazards and root causes.
- Communicate effectively to inform and educate.
- Strengthen, support and mobilize communities and partnerships.
- Create, champion and implement policies, plans and laws.
- Utilize legal and regulatory actions.
- Enable equitable access to services.
- Build a diverse and skilled workforce.
- Improve and innovate through evaluation, research and quality improvement.
- Build and maintain a strong organizational infrastructure for public health.
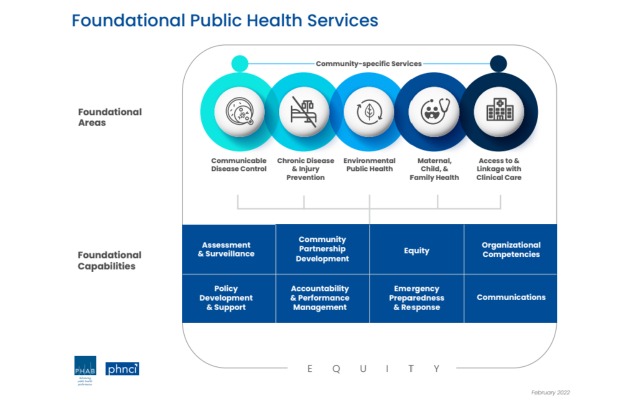
In addition, EPHS and PHAB domains reflect eight core public health capabilities:
Source: PHAB Standards & Measures for Initial Accreditation Version 2022
Equity is the linchpin of EPHS; better population health must benefit all communities. This means removing identified systemic and structural barriers like poverty, racism, gender discrimination and ableism.
3. Health departments report multiple benefits to accreditation
With the CHA at its core, PHAB standards work. CDC surveys confirm that health departments believe in the benefits of accreditation:
- stimulate quality improvement (95%);
- improve accountability and transparency (89%);
- strengthen relationships with key external partners (78%);
- use health equity to identify health priorities (73%); and
- strengthen resource utilization (68%).
4. The PHAB framework evolves as public health needs do
Established in 2007, PHAB is "the sole national accrediting body for public health in the U.S." Since 2011, its accreditation standards and measures have been updated three times with Version 2022 reflecting "the future of public health practice." In addition to fully aligning with the 10 EPHS, PHAB has embedded health equity in every domain and pandemic lessons learned in accreditation preparedness requirements.
5. All roads lead back to a strong CHA
Accreditation is not a one-and-done action. It is a continuous quality improvement effort that mirrors the aims of public health. Similarly, the CHA is not only an assessment but also a process. It’s a collaboration between those who conduct it and execute its findings, and one of the central pieces of documentation needed for PHAB accreditation.
Simplify your public health accreditation with DataGen
Want to learn more about how to simplify your Community Health Assessment for smoother PHAB accreditation? Contact us today to set up a free consultation specific to your organization’s needs.

.jpg)
Comments
Post a Comment